
Intervertebral disc disease (IVDD) is a degenerative disease process of the spine that can result in back pain and loss of mobility.
 What causes IVDD
What causes IVDD
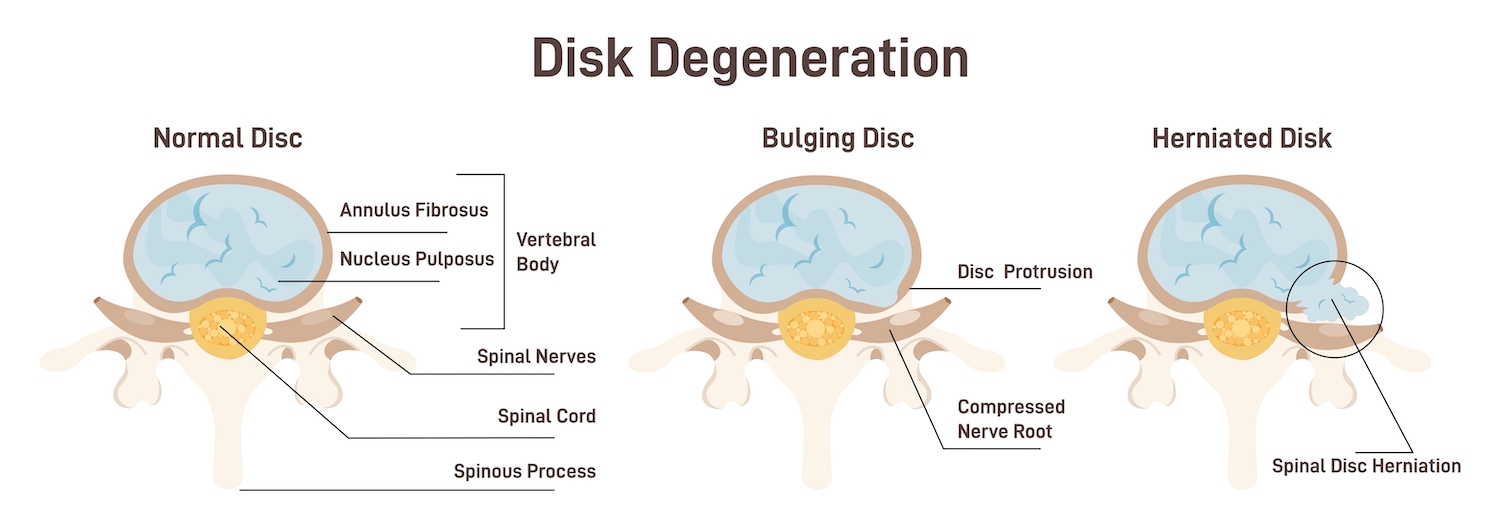
The intervertebral discs are the fibrous cartilage structure between the boney vertebrae of the spine. An intervertebral disc is composed of two parts with a structure similar to a jelly donut. (IVDD) is a degenerative disease process of the spine that can result in back pain and loss of mobility.
What causes IVDD
The intervertebral discs are the fibrous cartilage structure between the boney vertebrae of the spine. An intervertebral disc is composed of two parts with a structure similar to a jelly donut. The outer covering of the disk is a thick, tough, and fibrous shell called the annulus fibrosis. The annulus fibrosis is the outer chewy dough of the donut. The inner squishy middle of the disk is called the nucleus pulposus. The nucleus pulposus is the jelly center of the doughnut.
Intervertebral Disc Disease (IVDD) is an age-related degenerative process that affects the spinal cord of dogs. Degenerative disc disease causes deterioration of the outer annulus fibrosus, which can result in a bulging or herniation of the disc. The spinal cord is encased within the boney canal of the vertebrae and cannot move away from the pressure of bulging or herniating discs. Compression of the spinal cord results in pain and loss of neurologic function.
There are two types of intervertebral disc disease.
Type 1 – IVDD type 1 occurs in small dogs that have longer backs and short legs including dachshunds, corgis, basset hounds, Lhasa Apsos, Chihuahuas, toy poodles, French bulldogs, beagles, and Shih Tzus. The center of the disc herniates through a tear in the outer part of the disc, similar to jam bursting out of the donut. This is referred to as a herniated disk. A herniated disc causes acute compression of the spinal cord and can result in sudden onset of pain, difficulty walking, and paralysis.
Type 2 – IVDD type 2 occurs in large dogs such as labradors, Dobermans Pinschers, and German Shepherds. The fibrous outer layer of the annulus fibrosus starts to deteriorate allowing both the outer and inner parts of the disc to bulge out and compress the spinal cord. This is similar to a bulging donut. IVDD type 2 has a slow chronic onset and may be less painful. There may not be a particular moment or action that can be identified as having caused the damage.
Symptoms of IVDD
Intervertebral Disc Disease symptoms depend upon which part of the spine is affected and how severely the spinal cord is compressed. Symptoms of IVDD may appear suddenly or come on gradually.
Symptoms of Intervertebral Disc Disease (IVDD) may include:
• Holding the neck low or unwillingness to lift the head
• Hunched back and stiff appearance
• Avoidance of normal activities such as climbing stairs
• Shivering, panting, or crying due to pain
• Reluctance to move
• Unsteadiness or weakness in limbs
• Uncoordinated movements and difficulty walking
• Knuckling or dragging of paws
• Paralysis of limbs
• Urinary or fecal incontinence
If a dog is displaying any of the above symptoms, seek veterinary care as soon as possible. IVDD can be very painful for dogs and early treatment is essential for preventing the condition from becoming more severe. Delayed treatment may cause irreversible damage to the spine.
 Diagnosis of IVDD
Diagnosis of IVDD
Intervertebral disk disease is diagnosed based on clinical signs, exam findings, and imaging.
Physical Exam – A complete physical exam that includes neurologic and orthopedic evaluation should be performed by a veterinarian. Physical exam findings can help pinpoint the pain location along the spine.
Radiographs — Radiographs can identify evidence of disc degeneration, calcification, and narrowing of disk spaces. Other bone lesions such as cancers or infections that may cause similar symptoms to IVDD can also be identified on radiographs. However, because the spinal cord does not appear on X-rays, radiographs cannot definitively diagnose IVDD.
Magnetic resonance imaging (MRI) — A definitive diagnosis of IVDD is usually achieved with advanced imaging of the spine. An MRI can best diagnose IVDD because the image provides details of all the spinal structures and identifies the degree of spinal cord compression and the side affected.
Treatment for IVDD
The treatment for Intervertebral Disc Disease needs to begin as early as possible to achieve good treatment outcomes. Your dog to the vet for a full examination if you spot signs of IVDD. Delays in treatment could lead to irreversible spinal damage.
Anti-Inflammatory Medications
If a patient is diagnosed with a mild to moderate IVDD, treatment may include non-steroidal anti-inflammatory medications (NSAIDS) such as Carprofen, Deracoxib, or Meloxicam. Some patients may respond better to steroids such as prednisone or methylprednisolone to help reduce pain and swelling.
Pain medications and Muscle relaxers
Patients with moderate IVDD symptoms may benefit from Gabapentin, a medication that targets nerve-related pain. Many patients may be more comfortable if also prescribed muscle relaxers such as methocarbamol. Occasionally, patients with severe pain may be prescribed opioids such as codeine.
Activity Restriction
Patients suffering from IVDD should have strict rest imposed the first 4 weeks. Rest helps minimize the strain on the spine, intervertebral discs, and surrounding musculature.
Patients should be confined to a small well-padded area, such as a kennel, for the first 2 weeks to impose bed rest. Absolutely no running, jumping, climbing, or playing should be allowed. The patient should be carried or escorted outside on a short leash for supervised bathroom breaks.
The patient can begin to return to some minor physical activity gradually over the next two weeks. Start with brief leash walks multiple times a day. Patients should continue to be confined to a small area when they are not supervised. Activities such as climbing, jumping, and running should still be restricted.
Acupuncture & Physical Therapy
Several studies have shown that IVDD patients that have acupuncture and physical therapy added to their treatment plan recover faster and better. Stimulation of acupuncture points help the body release endorphins, norepinephrine, and anti-inflammatory mediators that relieve pain and help the body to heal itself naturally. Physical therapy helps IVDD patients to gain strength and mobility. Targeted exercises help to build muscle mass, regain stability, and recover range of motion, allowing patients to recover quality of life sooner.
Surgery
Surgery is typically recommended for dogs suffering from more severe cases of Intervertebral Disc Disease. Patients that are experiencing paralysis may need surgical decompression of the spinal cord, when rest and medication are not sufficient to reduce pain and symptoms. During surgery the disc material which is pressing onto the spinal cord and causing the IVDD symptoms is removed.
 Prognosis of IVDD
Prognosis of IVDD
The prognosis for dogs with IVDD depends on several factors including the severity of the clinical signs, the location of the spinal cord compression, how quickly the patient receives treatment, and initial response to therapy.
Patients that have mild symptoms and receive veterinary care within 24 hours will likely improve with noninvasive care including medication and rest. These patients have a good prognosis. However, IVDD is a degenerative disease, symptoms can reoccur and get worse over time. Patients that initially respond to noninvasive care may eventually need surgical intervention.
Patients that have severe or acute symptoms such as paralysis have a more guarded prognosis. Dogs with severe symptoms of IVDD that rapidly receive veterinary care, including MRI and surgery, within 24 hours have a 90% chance of regaining mobility and function. If veterinary care is delayed beyond 24 hours, the patient may only have a 50% chance of regaining normal function. If surgery is not successful in returning a pet to normal mobility, a dog wheelchair can help a dog to enjoy a happy and active life.






 Causes and Toxicity
Causes and Toxicity Clinical Signs
Clinical Signs Treatment
Treatment Prevention
Prevention
 Fleas are insects that consume blood from mammal hosts. Adult fleas are tiny, measuring only 2.5 mm long. Their bodies are shiny and reddish brown in color. Fleas do not have wings, but they can jump long distances. Several species of fleas can infest pets, but the most common one found on cats & dogs is the cat flea or Ctenocephalides felis. Fleas are a public health concern because they can
Fleas are insects that consume blood from mammal hosts. Adult fleas are tiny, measuring only 2.5 mm long. Their bodies are shiny and reddish brown in color. Fleas do not have wings, but they can jump long distances. Several species of fleas can infest pets, but the most common one found on cats & dogs is the cat flea or Ctenocephalides felis. Fleas are a public health concern because they can 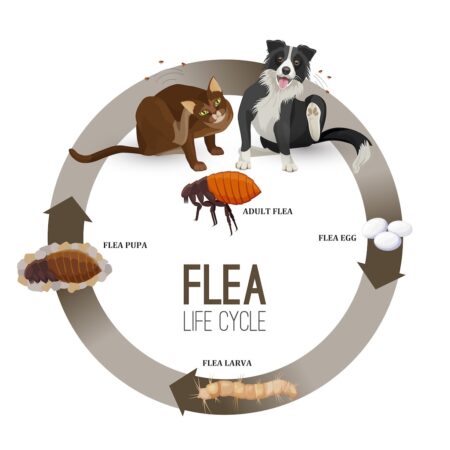 Flea Life Cycle
Flea Life Cycle Symptoms & Diagnosis
Symptoms & Diagnosis Prevention
Prevention 
 Symptoms of Feline Urinary Disease
Symptoms of Feline Urinary Disease Treatment of FLUTD
Treatment of FLUTD Improve Liter Box Accommodations
Improve Liter Box Accommodations Increase Water Intake
Increase Water Intake
 Causes
Causes Diagnosis
Diagnosis Follow-up
Follow-up
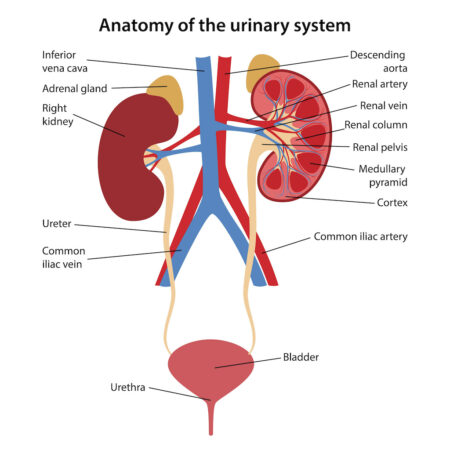 The kidneys are remarkable and complex organs that serves many essential functions.
The kidneys are remarkable and complex organs that serves many essential functions. Clinical Signs
Clinical Signs Urine Tests
Urine Tests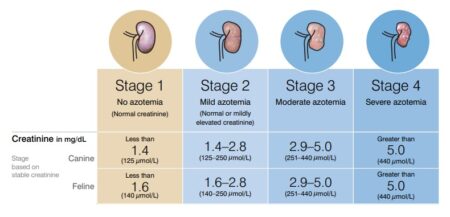
 Nutritional Therapy – Prescription therapeutic foods, such as Science Diet KD or Purina NF, are formulated with low levels of phosphorous and moderate amounts of high quality protein. These diets are highly palatable and calorie dense to support debilitated animals. Prescription renal diets have domonstrated in studies to prolong survival time, slow disease progression, and improved quality of life.
Nutritional Therapy – Prescription therapeutic foods, such as Science Diet KD or Purina NF, are formulated with low levels of phosphorous and moderate amounts of high quality protein. These diets are highly palatable and calorie dense to support debilitated animals. Prescription renal diets have domonstrated in studies to prolong survival time, slow disease progression, and improved quality of life. 
 No amount of chocolate is safe for an animal to ingest. The effects of chocolate consumption in pets depends on type of chocolate, quantity consumed, and the size (body weight) of the pet. Some types of chocolate contain higher amounts of caffeine and theobromine.
No amount of chocolate is safe for an animal to ingest. The effects of chocolate consumption in pets depends on type of chocolate, quantity consumed, and the size (body weight) of the pet. Some types of chocolate contain higher amounts of caffeine and theobromine. Treatment of Chocolate Toxicity
Treatment of Chocolate Toxicity
 Diagnostic Tests
Diagnostic Tests Treatment Options
Treatment Options Follow-up Care
Follow-up Care
Recent Comments